Are you tired all the time?
Do you wake up feeling exhausted and like you haven’t slept?
Have you fallen asleep at the wheel?
Does your significant other complain about your loud snoring?
Do others report that you stop breathing or gasp during sleep?
Are you just not feeling on top of your game?
If you answered yes to any of the above, read on!
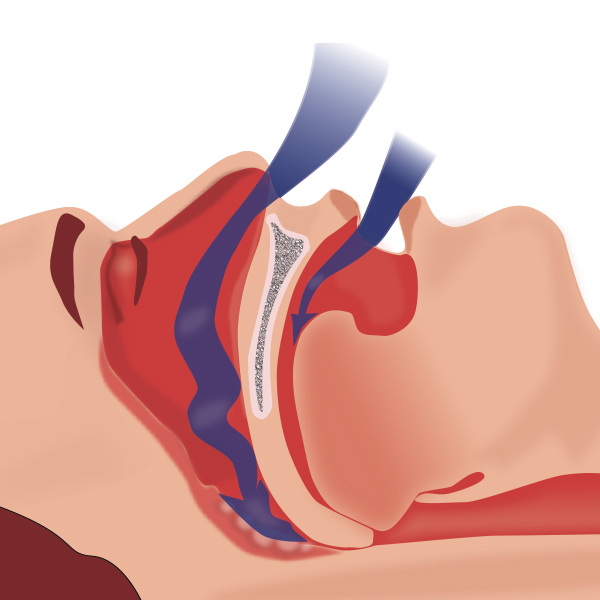
Sleep Apnea is a common and serious medical condition in which breathing is repeatedly interrupted during sleep. Sleep apnea occurs when the muscles in the back of the throat relax during sleep and fail to keep your airway open. Breathing interruptions may also be caused when tissue in the back of the throat, like the base of the tongue or tonsils and adenoids, partially or completely block your airway and reduce the amount of air that can reach your lungs (see below).
These airway blockages prevent your body from taking in enough oxygen, so blood (and brain) oxygen levels often fall to unsafe levels in people with sleep apnea. When oxygen levels drop, the brain responds by alerting the body, causing a brief arousal or awakening from sleep that re-establishes normal breathing. This situation results in the “snore-breathing pause-gasp” pattern typical in sleep apnea and often continues throughout the night (especially when sleeping on your back and in the early morning hours).
Current estimates are that 18 to 20 million Americans have sleep apnea, and approximately 80% of the population are undiagnosed. The condition is two to three times more common in men than in women; an estimated 20 to 30% of men between the ages of 30 and 70 have symptoms of sleep apnea.
Could you be one of them?
Here are some common factors that can put you at risk for sleep apnea:
- Obesity – especially an “apple” body shape
- Large collar size (17” in men, 16” in women)
- Large tongue
- A short lower jaw (compared to the upper jaw)
- Large tonsils/adenoids
- A family history of sleep apnea
- African-American race
- Environmental allergies and chronic nasal congestion
- Smoking
- Use of alcohol, sedatives or tranquilizers
Some common symptoms of sleep apnea include:
- Loud snoring or choking noises
- Pauses in breathing during sleep
- Waking up during sleep gasping for air
- Frequent urination at night
- Difficulty staying asleep
- Waking with a dry mouth or sore throat
- Morning headaches
- Excessive daytime sleepiness
- Lack of energy
- Irritability
- Difficulty paying attention
- Drowsiness while driving
If any doubt, check it out!
If you think you may have sleep apnea, you should tell your healthcare provider about your concerns because the consequences of undiagnosed or untreated sleep apnea are real, are serious and are preventable with appropriate treatment. They include:
- High blood pressure
- Heart disease and heart attacks
- Pre-diabetes and diabetes
- Stroke
- Reduced sex drive and erectile dysfunction
- Memory loss
- Cognitive problems
- Depression
In order to diagnose sleep apnea, your health care provider will arrange for you to have an overnight sleep study, which may be performed either in a sleep lab or in your home. Studies in a sleep lab involve a sleep technologist monitoring your breathing, heart rate, blood oxygen levels, body position and movements, and brain activity over the course of the night. Home studies usually collect a more limited amount of information focused on breathing and blood oxygen levels but the devices used are smaller, easier to set up, and allow you to sleep more comfortably in your own bed. Your healthcare provider will help decide which type of test is best for you.
Depending on the type and severity of sleep apnea, there are a number of well-established and effective options for treatment. Your healthcare provider will discuss these with you and recommend the most appropriate course.
The most common treatment for sleep apnea is Positive Airway Pressure (Continuous=CPAP; Bi-Level=BiPAP). Using PAP involves wearing a small facial “mask” (there are many different types) with a lightweight hose that is in turn attached to a compact machine (also of many types) that creates air pressure. The air pressure flows through the nose and/or mouth, depending on the type of mask worn, and helps hold the airway open so you can breathe normally during sleep. While you may have heard about difficulties that others have had getting used to PAP, many patients adapt to using the machine nightly, especially once they realize how much better they feel. Having an adjustable (“Auto-PAP”) machine with heated humidification and a gradual increase in pressure may help a lot!
Other treatment options include oral (dental) appliances and surgical procedures if the obstruction is caused by tissue blockages that can be surgically corrected. Even a modest amount of weight loss can also make a big difference, as can stopping smoking and avoiding sleep apnea triggers like alcohol.
The Game Plan: If you have sleep apnea, get diagnosed/treated. You owe it to your family, your team and yourself.
Additional Resources:
National Sleep Foundation: www.sleepfoundation.org
MyApnea.Org: www.myapnea.org
American Sleep Apnea Association: www.sleepapnea.org
American Academy of Sleep Medicine Educational Website: www.sleepeducation.org
Harvard Sleep and Health Education Program: healthysleep.med.harvard.edu/portal